Sleep Guide for People with Special Needs, Disabilities
by | Last Updated
People with disabilities often have difficulties performing everyday activities without special care or special equipment.
When it comes to sleep, which is one of our basic everyday needs, it is no different. Whether the disability involves pain or not, it can make it difficult to get enough quality sleep. And a lack of sleep, in turn, may result in sleep disorders and a number of very serious, life-threatening health conditions.
So, in order to get their portion of a good night’s sleep, each person with a disability should understand the sleep problems associated with their particular condition and know how those problems can be solved.
This could take a lot of research, given the fact that each disability may affect one’s life differently. That’s what this guide is for. Hopefully, it will help the disabled — and those who care for them — get a better understanding of their sleep needs and ways to fulfill these needs properly.
Disabilities and Sleep: Overview and Statistics
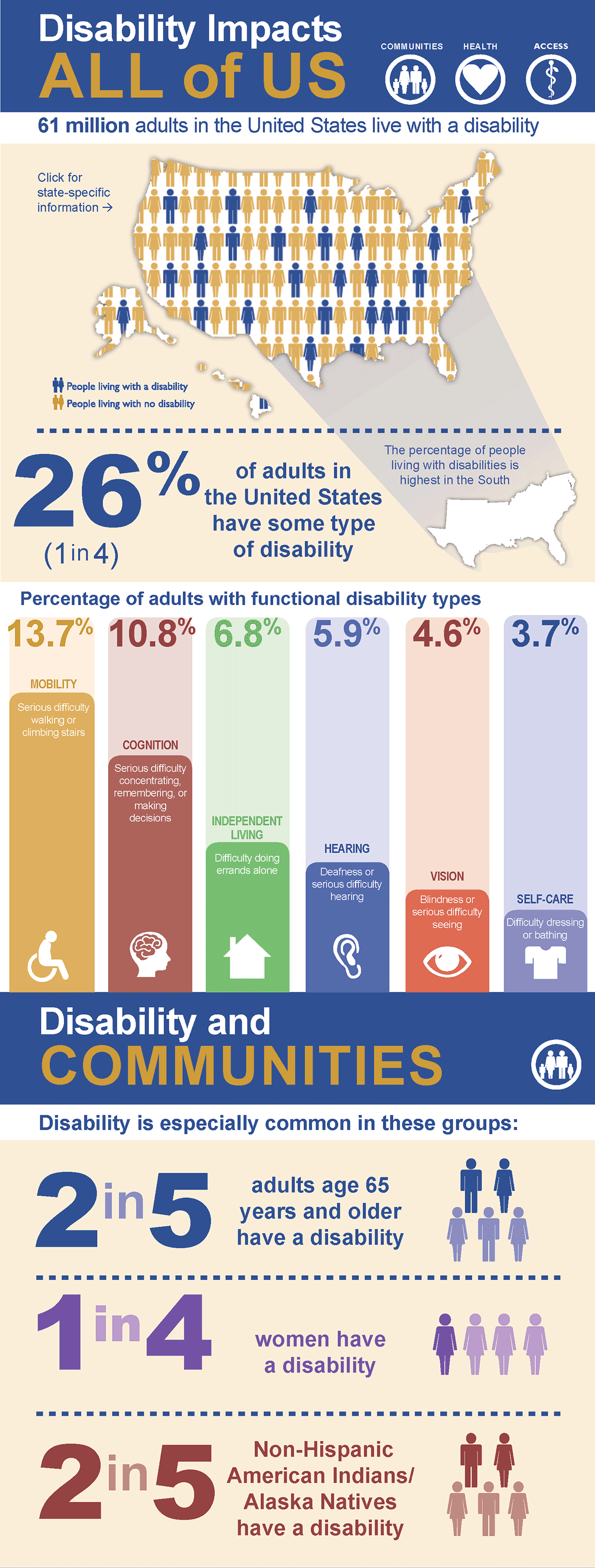
Source: cdc.gov
According to the most recent data from the U.S. Census Bureau, there were nearly 85.3 million people with disabilities in America in 2014, which made up 27.2% of the population. It is much more, compared to the previous data from 2010, when there were 56.7 million disabled (19%). So, one may suggest that today the numbers are even higher.
The 2017 Disability Statistics Annual Report states that 24.8% of U.S. adults have an ambulatory disability, meaning that they’re able to perform simple tasks or even get a job. However, if the employer doesn’t provide disabled people with proper working conditions, this may result in stress and poor sleep. And there are lots of other factors making it difficult for disabled people to fall and stay asleep (we’ll discuss them below).
Speaking of sleep, the statistics aren’t very encouraging here either. According to data from the Gallup poll, the average sleep duration decreased over the past 50 years from 7.9 hours per night in 1942 to 6.8 hours in 2013. Researchers link this to the industrialization process, but the change is still pretty dramatic.
Insomnia is the most common sleep disorder, as it affects 30% of Americans, with 10% of them being chronic insomnia sufferers. According to a study conducted by researchers at the University of Wisconsin, chronic insomnia often correlates with adverse health effects, which include cardiac morbidity, depressive disorders, and obstructive sleep apnea. And these conditions may actually increase the risk of getting a disability as a result of stroke or heart attack.
As you can see, there’s a link between sleep disorders and impairment, which means that they can influence each other. Thus, treating sleep issues may help improve the overall condition of a disabled person.
Sleeping with Disabilities — Why Does It Get So Difficult?

When a person’s life is affected by disability, it may change the perception of habitual things, and sleep is one of them. Typically, people with disabilities have difficulties with falling asleep because of the following reasons:
- Pain. Many of the medical conditions defined as disabilities cause pain. For example, systemic lupus or inflammatory arthritis. And sleeping with pain, especially if it becomes chronic and strikes you every night, is not easy. And the tricky thing is, disabled people may express their complaints about pain differently than non-disabled. For example, they might not have a standard pain grimace due to facial paralysis or altered mimic. That’s why caregivers should pay special attention to learning about how their ward expresses the pain, and address these expressions.
- Anxiety. Anxious thoughts and constant stress are common in people with disabilities. If neglected, they may gradually turn occasional sleepless nights into chronic insomnia.
- Sleep associations. This problem is more common in children and adolescents. For example, children with autism very quickly become attached to certain rituals. If their bedtime routine involves watching TV on a sofa, they may begin to fall asleep on it, so their bedroom won’t be viewed as the place for sleep anymore.
- Medication side effects. Disabled people often need to take a lot of different medications to alleviate their symptoms. Some drugs may interfere with sleep quality, duration, or structure, thereby making sleep less restorative.
- Disrupted circadian rhythms. Visually impaired people or individuals with ADHD and autism may have difficulty falling asleep at the usual time. Blind people aren’t familiar with light and darkness cycles, so their internal clock is initially disrupted. Children with ASD have trouble reading social cues, so they may not recognize that it’s time to go to bed. These are just a few examples.
Physical Disabilities and Sleep
Source: tcdc.gov
Physical disabilities affect the functioning of a person’s musculoskeletal system and physical abilities.
Examples of physical disabilities include:
- Amputation. The Amputee Coalition claims that approximately 185,000 amputations occur in the United States each year. The leading causes of limb removal are vascular pathologies (diabetes and peripheral arterial disease) and traumas that led to limb loss.
- Cerebral palsy. Approximately 10,000 babies born each year have cerebral palsy. This is a congenital condition caused by non-progressive brain trauma during fetal development.
- Polio, or poliomyelitis. This infectious disease is caused by poliovirus. The main symptoms are weakness and dystrophy of leg muscles (mainly), but it can also affect diaphragm and neck.
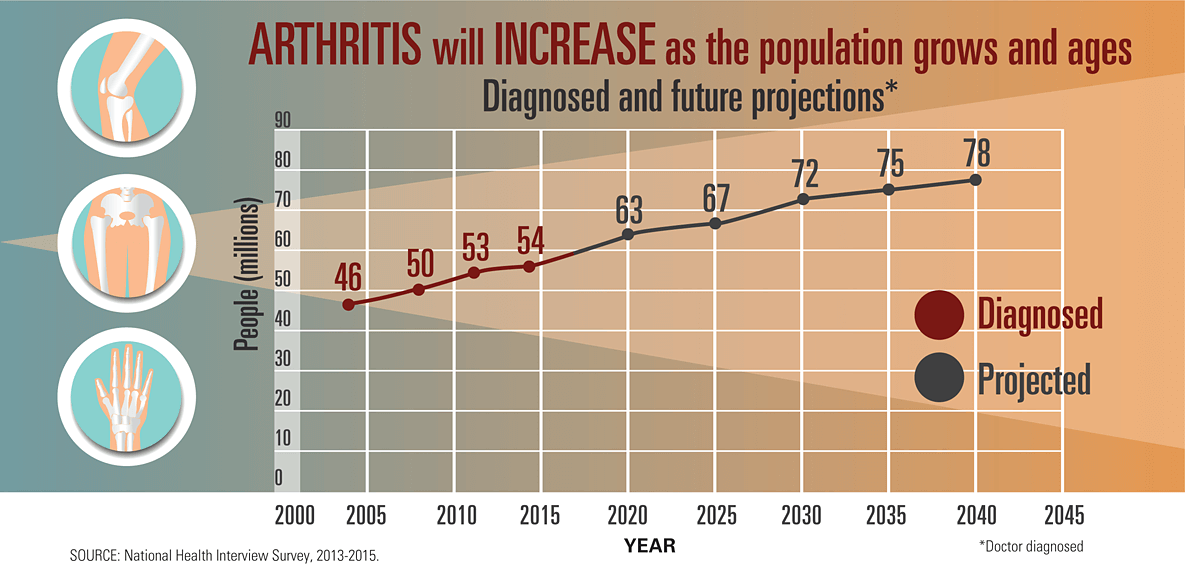
- Arthritis. The main symptoms of arthritis are joint inflammation and stiffness, which, in severe cases, can lead to complete immobilization. The most common type of arthritis is osteoarthritis: according to the estimates, 12.1% of the US population over 25 years old may have it.
- Spinal cord injury (SCI). Spinal cord injury may affect muscle function, sensitivity, or autonomic functions in parts of the body that are located below the level of damage. The National Spinal Cord Injury Statistical Center reports that about 17,500 new cases of SCI happen each year with the most common reason behind them being car accidents.
Sleep Problems in People with Physical Disabilities
The effect of physical disabilities on sleep quality is perhaps the most potent, and not because of pain episodes. Accidental disability, such as limb loss or spinal cord injury, puts a significant toll on a person’s psychological health. Disability is known to be a risk factor for depression, as disabled people are exposed to a lot of stressful factors:
- they need to switch their social roles or completely give up their social life;
- they become more exposed to abusive behavior from other individuals;
- they encounter the lack of inclusivity and proper healthcare.
All these factors may impact sleep quality and lead to the following sleep issues:
- Insomnia. Pain and spasms are the main reasons behind insomnia in physically disabled individuals. More than 70% of people with chronic musculoskeletal pain reported moderate to severe insomnia symptoms that last through the night. Also, 95% of patients that went through amputation surgery reported experiencing painful episodes, such as phantom limb pain or residual limb pain.
- Sleep apnea and excessive daytime sleepiness. Individuals with muscle dystrophy may experience sleep apnea episodes, which can lead to daytime drowsiness.
- Bruxism. Bruxism involves involuntary teeth grinding or jaw clenching during the night. This sleeping disorder affects 8-16% of adults and up to 20% of children. Those with cerebral palsy are more likely to have bruxism spasms than people not affected by CP.
Excessive drooling is common among children with cerebral palsy and may pose a threat to their lives by creating a choking hazard.
Sleep Advice for People with Physical Disabilities
Sleep disorders in physically disabled people require a complex approach to physical problems as well as the creation of inclusive surroundings for everyday life:
- Eliminating pain. The use of pain-killing medications or therapy for patients with an amputation will help cope with pain issues and get better sleep.
- Creating supportive surroundings. Depending on each unique situation, a person shouldn’t have difficulties with getting up or moving around the bed. Caregivers may opt for low-profile beds or adjustable bed bases, which allow creating a slight incline instead of lying flat. Paralyzed individuals may need additional bed handles to hold on while moving from a wheelchair to bed, or rails that would prevent them from falling during sleep.
- Using alternatives. Along with traditional medicines, people with physical disabilities can benefit from alternative treatment options, such as acupuncture or herbal sleeping aids that don’t have habit-forming mechanisms.
- Changing lifestyle. If a disabled individual can move a bit, it’s recommended to support the level of feasible activity throughout the day. Exercising can help blow off some steam and provide a disabled person with endorphin boost that can positively impact their sleep.
Before implementing any changes to current treatment, a disabled person or their caregiver should address their ideas to a profile healthcare practitioner.
Sensory Disabilities and Sleep
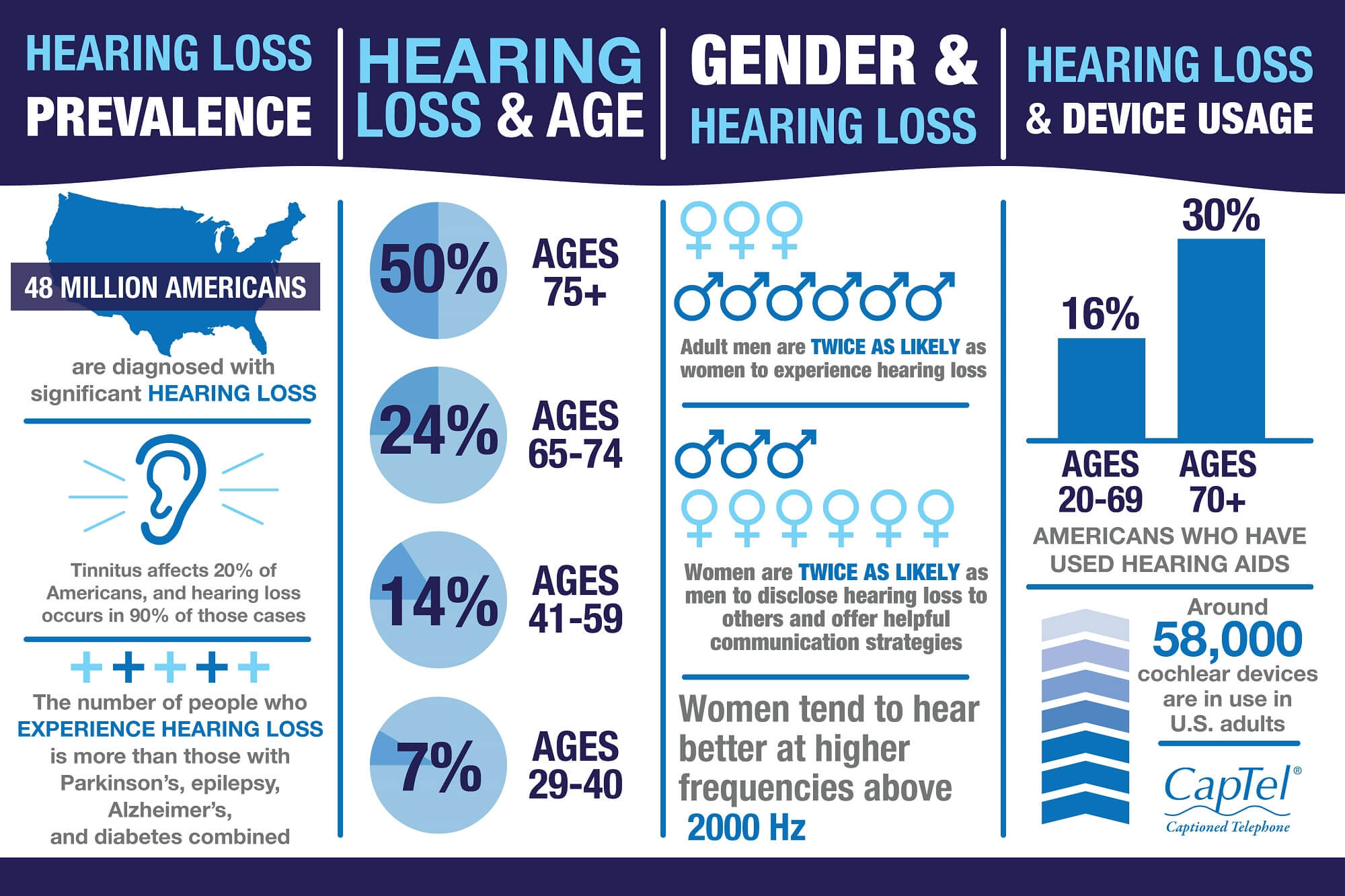
Source: captel.com
A sensory disability affects how a person gathers information from the world around them. The examples of sensory disabilities include:
- Deafness, or poor hearing. Hearing loss is the third most prevalent chronic condition in older adults, along with hypertension and arthritis. Every fourth person at the age of 65-74 years has some degree of deafness.
- Blindness, or vision loss. According to the data from the 2016 American Community Survey, more than 7 million adults had some type of vision disability.
- Autism spectrum disorder (ASD). Typically, ASD manifests in early childhood with the main signs being avoiding eye contact, not reacting to the name, and avoiding the company of other kids. According to recent estimates, up to 80% of young autism patients deal with regular sleep issues.
- Sensory processing disorder (SPD). SPD is often confused with ASD, but in fact, they don’t always accompany each other. SPD affects the ability to adequately react to sensory stimuli, e.g. bright lights, noises, colors, smells, and textures. According to the American Occupational Therapy Association, about 5% of kids have SPD.
Sleep Problems in People with Sensory Disabilities
A sensory disability can affect how the person gathers information from the world around them. Examples of sensory disabilities include:
- Deafness, or poor hearing. Hearing loss is the third most prevalent chronic condition in older adults, along with hypertension and arthritis. Every fourth person at the age of 65-74 years has some form of deafness.
- Blindness, or vision loss. According to the data from the 2016 American Community Survey, more than 7 millions of adults have some form of vision disability.
- Autism spectrum disorder (ASD). Although it is too complex to categorize it as a sensory disability, people affected by this disorder often experience sensitivity to sensory stimuli. Typically, ASD manifests in early childhood with the main signs being avoiding eye contact, not reacting to the sound of the name, and avoiding the company of other kids. Experts estimate that up to 80% of young autism patients deal with regular sleep issues.
- Sensory processing disorder (SPD). SPD is often misled for ASD, but in fact, it can occur without the presence of autism disorder. This disorder affects the ability to adequately react to sensory stimuli, e.g., bright lights, noises, colors, smells, and textures. American Occupational Therapy Association states that about 5% of kids may have SPD.
Sleep Problems in People with Sensory Disabilities
Sleep issues in sensory disabled people are strictly connected to their perception difficulties.
For example, blind people have no light perception, which means that they go out of sync with their circadian clock and may develop non-24-hour sleep-wake disorder (non-24). They have difficulty falling asleep at the usual time, and their sleep-wake cycle is often unbalanced.
Deaf individuals can suffer from tinnitus, a high-pitched sound that comes from the inside of the body. Although tinnitus isn’t a sleep disorder, it can result in headaches, sleep shortage, and insomnia, which directly affect the quality of a person’s shut-eye.
Children with autism, as well as those with SPD, can get overly anxious before sleep or have vivid dreams in the middle of the night, which can contribute to sleep terrors and frequent awakenings. Also, autistic kids are more prone to snoring and sleep apnea.
Sleep Advice for People with Sensory Disabilities
Addressing sleep-related issues in sensory disabled people aims towards encouraging a healthy lifestyle and creating a sleep-friendly space that will promote restful sleep despite sensory issues:
- Using a white noise machine. White noise can absorb the surrounding sounds, including ringing ears, and promote deep sleep. Another ‘colorful’ noise that helps combat insomnia is pink, and studies suggest that it may even have memory-improving properties.
- Buying a weighted blanket. Both kids and adults with sensory disorders often cannot sleep because of anxiety and stress. A weighted blanket can resemble a hug and provide the disabled person with a comforting feeling.
- Limiting caffeine. Caffeine, especially if taken during the evening hours, can boost alertness levels and disrupt sleep even more, which is especially undesirable for those with non-24. Also, people with sensory disabilities can have a more pronounced physiological reaction to caffeine than non-disabled individuals.
As it is known, people with limited ability to use one of the senses may develop a larger brain capacity to process information through other senses. Thus, both blind and deaf people may benefit from aromatherapy, e.g. by placing lavender sachets near their bed. This scent has proven to have a calming effect.
Also, deaf people and those with hearing problems, particularly kids, may find it a good idea to use a nightlight in their room so that the absence of sound wouldn’t trigger anxiety.
Alcohol is another substance to be avoided by people with any disabilities. Even though alcohol beverages act as a depressant and may promote sleepiness, they cut out the percentage of REM sleep in the second part of the night, which results in poor sleep quality.
Mental Disabilities and Sleep

Mental disorders are chronic conditions that affect a person’s life and relationships. To be considered as a disability, a mental disorder must:
- interfere with a person’s ability to perform everyday tasks;
- adversely affect work performance;
- make a person unable to function without a caregiver.
Also, a person should have a documented history of the treatment of a mental disorder for at least 12 months.
Sleep Problems in People with Mental Disabilities
The most frequent complaint in individuals with mental disabilities is insomnia: up to 80% of schizophrenia patients report the symptoms. People with major depression and bipolar disorder may develop chronic insomnia in 50% of cases, depending on the severity of the depressive episode.
Contrary to insomnia, hypersomnia is the urge to sleep more than needed and excessive sleepiness during daytime. This condition is prevalent among people with such mental disabilities as severe depression or schizophrenia.
People with mental disorders are more prone to nightmares and lucid dreams, which can impact sleep duration and overall quality.
Since one of the causes of mental disorders is a chemical imbalance in the brain, they can also affect circadian rhythms and make them go out of sync. This can result in delayed phase sleep disorder, non-24-hour sleep disorder, and so on.
The use of medications, such as antidepressants and antipsychotics, may alter the sleep structure and thus make sleep less restorative.
Sleep Advice for People with Mental Disabilities
The treatment of sleep issues in people with mental disabilities varies depending on the type of disorder. General recommendations usually include:
- Scheduling psychotherapy sessions. This could be either cognitive-behavioral therapy, psychoanalysis, or other forms of dialogue.
- Addressing symptoms. The use of certain medications can help minimize the symptoms of mental illness and improve the quality of life, which will contribute to better sleep.
- Implementing lifestyle changes. Sleep routine and scheduled physical activity of any kind may help balance the chemicals in the brain and aid in getting proper sleep.
Complementary medicine and herbal remedies can also be used as part of the complex therapy of sleep issues in mentally disabled patients.
Intellectual Disabilities and Sleep

Intellectual disabilities affect a person’s ability to learn and process information and interfere with social and communication skills. They are typically diagnosed during the first years of life. Examples of the most common intellectual disabilities include:
- Down syndrome. This is a genetic pathology caused by the mutation in 21 chromosomes. One out of every 700 babies in the US are born with Down syndrome, which makes it the most common chromosomal disorder in America.
- Attention Deficit Hyperactivity Disorder (ADHD). According to the data from the Neurotherapeutics Journal, ADHD may affect from 5.9 to 7.1% of children and adolescents.
- Fetal Alcohol Syndrome (FAS). This syndrome affects children who were exposed to alcohol during fetal development. The National Organization on Fetal Alcohol Syndrome reports that approximately 40,000 newborns each year are affected by FAS.
Sleep Problems in People with Intellectual Disabilities
Along with already mentioned sleep issues, individuals with intellectual disabilities may suffer from the following problems:
- Restless Leg Syndrome (RLS). Repetitive and sharp movement and unpleasant sensations can lead to sleep disruptions in disabled people. Some studies found that ADHD, periodic limb movement syndrome and RLS may co-occur.
- Obstructive sleep apnea (OSA). OSA is highly prevalent in people with Down syndrome. They typically have low-set cheekbones, short jaws, and narrow airways that are more prone to collapsing. Their disability also increases the chances of developing obesity, which is another risk factor for sleep apnea.
- Anxiety-induced insomnia. Children with fetal alcohol syndrome are very sensitive sleepers. Since their central nervous system is underdeveloped, they may have problems with emotional regulation and are more prone to insomnia.
People with severe cognitive impairment may not get the idea behind the change of night and day, just like newborn babies. They can become overly active at night and sleep through the day, which results in poor sleep not only for them — because daylight disrupts their shut-eye — but for their caregivers as well.
Sleep Advice for People with Intellectual Disabilities
Improving sleep in people with intellectual disabilities comes down to creating comfortable surroundings that will soothe them to sleep. The main recommendations for caregivers and family members include the following:
- Using a waterbed. Waterbeds are great when it comes to creating a soothing surface for sleep. They adapt to body curves and support neutral body temperature throughout the night. Also, waterbeds eliminate the risks of developing bed sores and ulcers during sleep.
- Referring to CPAP machines. For alleviating sleep apnea symptoms and improving sleep quality people with intellectual disabilities may need CPAP therapy.
- Investing in a firm mattress. A firm mattress can offer better support for overweight people and help them get proper sleep.
- Using white noise machine. White noise provides a soothing sound that may distract overly sensitive people with ADHD or FASD from clock ticking, fans, tap water, or other unpleasant sounds.
Additional Information
- The National Down Syndrome Society offers healthcare guides for children and adults with DS.
- The Anxiety and Depression Association of America has an online peer-to-peer group, where people can ask questions and share tips on how to get better sleep.
- non-24.com contains all the info about living with Non-24-Hour sleep-wake disorder and has many useful sleep tips.
- The Hearing Health Foundation can help people learn more about hearing loss and interventions that help deaf people live a healthy life.
- The Cerebral Palsy Guidance is a useful resource for people who take care of individuals with cerebral palsy. Contains a lot of helpful info on how to integrate people with CP into society.
- The Arthritis Foundation provides the latest data about arthritis and its treatment and offers state programs to help people with arthritis as a volunteer.
- The Disability Foundation is a non-profit project that helps people with physical disabilities regain motivation and reintegrate into a healthy life.





No Comments